SURGERIES AND TREATMENTS
Bone-anchored hearing aids
Types, Benefits and What to Expect

By Joe Saliba, MD | Neuro-otologist and Skull Base Surgeon
Key Highlights
- Bone anchored hearing devices transmit sound through bone conduction, bypassing the outer and middle ear to directly stimulate the inner ear (cochlea).
- They differ from conventional hearing aids by offering a solution when traditional amplification is ineffective, such as in cases of conductive or mixed hearing loss, or single-sided deafness.
- There are two main types: percutaneous systems (with an abutment through the skin) and transcutaneous systems(with an internal magnet under intact skin), each with specific advantages and limitations.
- Hearing outcomes are excellent when patients are properly selected, but potential complications such as skin infections or magnet pressure issues must be considered.
- MRI compatibility and artifact considerations are critical when choosing the device, especially for patients who may need brain imaging in the future.
- Proper care and maintenance of the device and implant site are essential to ensure optimal performance and minimize complications over the long term.
Bone-anchored hearing aids (BAHAs) are specialized devices designed to help individuals with specific types of hearing loss who may not benefit from traditional hearing aids. They bypass damaged parts of the ear and using bone conduction to simulate the inner ear directly. These implants are surgically implanted and offer a unique solution for improved hearing. Below, we’ll explore how they work, their differences from conventional aids, clinical uses, types, outcomes, and care tips.
What are bone-anchored hearing aids?
Bone-anchored hearing aids (BAHAs) are surgically implanted devices that transmit sound through vibrations in the skull bone directly to the inner ear. Unlike conventional hearing aids, which amplify sound through the ear canal, BAHAs skip the outer and middle ear entirely. This makes them ideal for people with conductive hearing loss (e.g., ear canal malformations, chronic infections) or single-sided deafness.
How do they work?
The concept behind bone anchored hearing aids lies in something called bone conduction. Normally, sound waves travel through the outer and middle ear to reach the inner ear. In cases where the outer or middle ear is damaged, malformed, or chronically infected, sound cannot reach the cochlea effectively and normal hearing aids won't work.
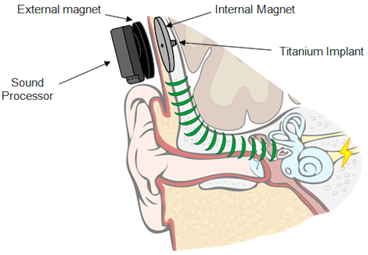
BAHAs take advantage of the skull's natural ability to conduct sound vibrations. Here is a summary of how they work:
- Implant: A small titanium implant is fixed into the skull (usually behind the ear). The implant needs to fuse with the bone (process called "osseointegration") before it can be used, which can take 1-3 months after the surgery. To learn more about the surgery for bone-anchored hearing devices, read this article.
- Sound processor: A sound processor (outside device that connects to the titanium implant either directly or through a magnet) captures external sound with a microphone, converts it into mechanical vibrations.
- Bone conduction: These vibrations are transmitted through the bone of the skull directly to the cochlea (inner ear), bypassing damaged outer/middle ear structures.
- Hearing: The cochlea then processes the vibrations into nerve signals, allowing the brain to perceive sound.
This direct pathway ensures clearer sound transmission. The image below summarizes the step we just described:

How are they different than "standard" hearing aids?
- Sound pathway: Standard aids are worn in the ear and amplify sound through the ear canal, while BAHAs use bone conduction by vibrating the skull behind the ear (there is no device that goes in the ear canal in a BAHA).
- Comfort: BAHAs do not cause any ear canal blockage, reducing discomfort and feedback (whistling) from the device. There is also no issue with wax buildup or ear infections with a BAHA because the ear canal remains open.
- Eligibility: Standard hearing aids are less effective for individuals with physical ear malformations, chronic infections, severe conductive loss and single-sided deafness. Bone anchored hearing aids offer a direct, often clearer pathway for sound in these cases. For example, someone with aural atresia (absent ear canal) cannot be fitted with traditional aids but benefit from a BAHA. In my experience, I find that BAHAs are an excellent choice for individuals with single-sided deafness.
Here is a table that summarizes the differences:
| Feature | Bone Anchored Hearing Aids | Classic Hearing Aids |
|---|---|---|
| Sound Transmission | Via bone conduction | Via air conduction |
| Ear Canal Use |
Bypasses the ear canal entirely |
Requires an open ear canal |
| Indications |
Unable to fit a classic hearing aid, single-sided deafness, severe mixed hearing loss |
All types hearing loss as long as ear can be fitted |
| Surgical Requirement | Surgical implant (percutaneous or transcutaneous) | No surgery needed |
| Occlusion Effect | None | Potential occlusion (blocked ear feeling) |
|
Risks |
Surgical complications |
No surgical risks |
Who can qualify for a BAHA? (Clinical indications)
Bone anchored hearing aids are considered for patients who usually fall in one of those four categories:
-
Conductive hearing loss not correctable by surgery: Where the outer and/or middle ear prevents normal sound transmission, but surgery is not possible. Examples include: ossicular chain problems that failed prior reconstruction, ear atresia (where there is no ear canal) and severe malformations of the ear.
-
Mixed hearing loss not correctable by surgery: Where both conductive and sensorineural components are present, but the inner ear function is relatively preserved. These patients may have failed a prior surgical attempt or had many prior surgeries (example: severe otosclerosis operated in the past).
-
Chronic ear infections (unfit for classic hearing aids): Conditions that prevent the use of conventional hearing aids (e.g., chronic ear drainage).
-
Single-Sided Deafness (SSD): Patients with profound hearing loss in one ear and normal hearing in the other can use a BAHA to transmit sound from the deaf side to the good ear via bone conduction (bypassing the non-functional cochlea).
*** Important: Preoperative evaluation in audiology is required to confirm if a patient qualifies for a BAHA. This often includes a bone conduction hearing test and a trial with a bone conduction headband (a headband with a skull vibrator that replicates a BAHA) to predict benefit. The trial period is critical to make sure the patient benefits from the BAHA before performing a surgical procedure.
Types of bone-anchored hearing devices
There are two main types: percutaneous and transcutaneous systems.
1. Percutaneous Models (implant goes through a skin opening)
-
Example: Ponto by Oticon Medical
- How It Works: A titanium post (called abutment) extends through the skin (always sticks out and is visible), and the external sound processor clips directly onto the abutment. Even when the sound processor is removed (at night for example), the titanium post always sticks out (about 3 mm usually, so quite small). The post sticking out does not cause any harm to your skull.


-
Advantages:
-
The device connects directly to the bone, allowing sound to be transmitted efficiently with very little energy lost in the process.
-
Better sound transmission and higher amplification possible.
- Very easy surgery (I perform them under local anesthesia with a duration of approximately 15 minutes).
-
-
Disadvantages:
-
Risk of skin infections around the post that sticks out of the skin.
-
Requires daily cleaning and care around the implant site.
-
A visible metallic post, which some patients find cosmetically undesirable.
- Feedback (whistling) can occur if objects rub on the sound processor (hair, scarf, etc.)
-
2. Transcutaneous Models (implant is entirely under the skin)
-
Example: Osia by Cochlear
- How It Works: The implant sits entirely under the skin (nothing is visible on the outside when the processor is not worn). The sound processor attaches magnetically over the implant site, and sound is transmitted via magnetic coupling and radiofrequency antenna. In other words, you still need an external sound processor to hear, but when you remove it, there is no visible implant going through the skin.

-
Advantages:
-
No permanent skin opening—reduces infection risk.
-
Better cosmetic appearance.
-
Less maintenance at the implant site.
- No feedback even if objects rub on the sound processor.
-
-
Disadvantages:
-
Slight energy loss through the skin and soft tissues.
-
May not be powerful enough for severe mixed losses compared to percutaneous models.
-
Involves more complex internal hardware (especially in active transcutaneous systems like Osia).
- Requires a slighty more complex surgery (I perform them under sedation, duration is typically around 45 minutes).
-
Hearing outcomes and potential complications
Hearing Outcomes
Studies consistently show that bone anchored hearing aids significantly improve sound clarity, speech understanding, sound localization, and overall quality of life for properly selected candidates. Benefits are even more so in noisy environments and for overcoming unilateral hearing loss.
Potential Complications
-
Skin reactions: Common around the percutaneous abutment site (in percutaneous models).
-
Loss of implant: Failure of integration in the bone (rare).
-
Soft tissue overgrowth: Skin (and inflammatory tissue like granulation) can grow over the abutment, requiring revision surgery. This is only for the percutaneous model.
-
Pain or discomfort: At the implant site.
-
Device failure: Processor issues are rare but possible.
MRI compatibility
MRI compatibility is an important consideration for patients with bone anchored hearing aids.
- Percutaneous devices (like the Ponto system) typically involve a titanium implant without any internal magnets, making them generally MRI-safe up to 3.0 Tesla, though the external sound processor must be removed before imaging.
- Transcutaneous devices (like the Osia system) contain internal magnets that can pose challenges during MRI. Some transcutaneous systems are MRI-conditional, meaning scans can be performed under specific conditions (usually up to 1.5 Tesla) with careful preparation. Even when MRI is technically allowed, the magnet creates a "signal void" or artifact on the MRI images. This appears as a large black area around the magnet site, which can obscure critical structures in the head and neck, including parts of the brain. The size of the artifact varies depending on the magnet strength and the MRI sequence used, but it can significantly limit diagnostic imaging near the implant. If critical areas need to be evaluated (e.g., for tumors, multiple sclerosis, or other neurologic conditions), the artifact caused by the magnet will prevent accurate diagnosis. In these cases, a percutaneous device may be preferable because it produces less interference with imaging. Alternatively, some transcutaneous systems allow for magnet removal surgery before a major MRI, but this involves an additional procedure. When counseling patients, it’s important to assess the likelihood of future MRI needs to help guide the choice of implant.
Care of a Bone Anchored Hearing Aid (Patient Instructions)
For Percutaneous Systems (like Ponto):
-
Daily cleaning around the abutment using a soft brush and cleaning solution to prevent skin infections.
-
Inspect the skin regularly for redness, swelling, or discharge.
-
Keep the area dry and free from hair entanglement.
-
Remove the sound processor when swimming or showering.
For Transcutaneous Systems (like Osia):
-
No need to clean an external abutment.
-
Ensure the external processor's magnet strength is appropriate—not too tight to avoid skin irritation.
-
Maintain the external processor by wiping it gently and keeping it dry.
General Tips for All Users:
-
Schedule regular ENT or audiology check-ups to monitor implant and hearing function.
-
Handle the external processor carefully to prevent mechanical damage.
-
Be aware of warranty and servicing options for the sound processor.
Final thoughts
Bone-anchored hearing aids offer a life-changing solution for those with specific hearing challenges. By leveraging bone conduction, they provide clearer sound without the limitations of traditional aids. While surgical options require careful consideration, the benefits-improved communication, comfort, and safety-make them a valuable tool in hearing rehabilitation.
Joe Saliba, MD
Dr. Joe Saliba is an ENT surgeon specialized in neuro-otology and medical director at ODYO. He treats patients with various ear and skull base disorders, ranging from hearing loss and vertigo to vestibular schwannomas and cochlear implants.

A hearing test conducted by an audiologist is the first step towards achieving good hearing.
ODYO partners with audiology clinics to conduct comprehensive hearing assessments and create personalized intervention plans, specifically tailored to meet each patient's unique communication and hearing care needs.
